🧠 Sohar Health: AI-powered eligibility checks, VoBs and insurance discovery for behavioral health
Unleash your behavioral health company's potential with targeted eligibility verification, and AI-powered Verification of Benefits (VoB) to drive revenue from health payers.
⚡TL;DR
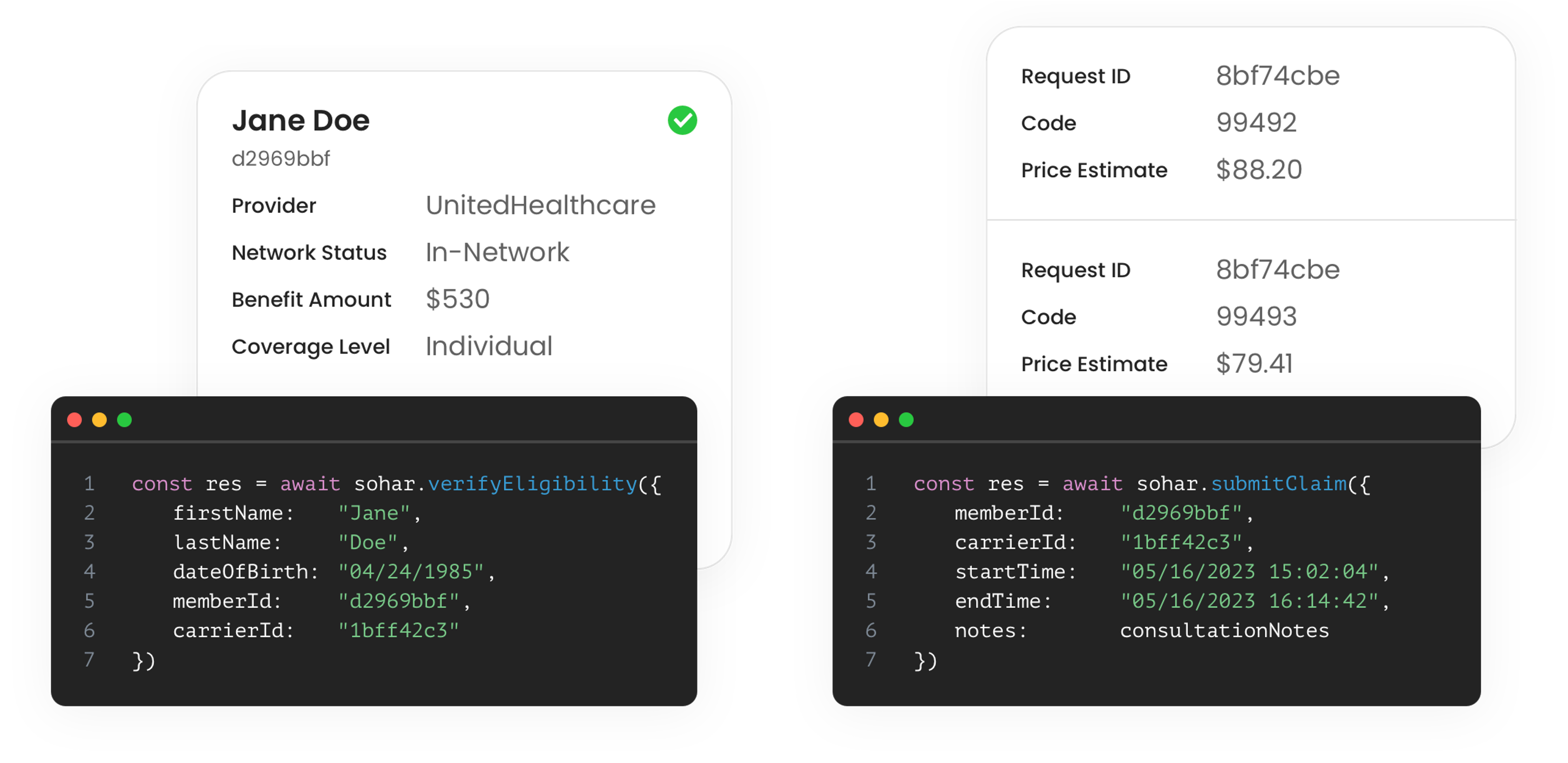
Behavioral health providers are investing significant resources into expensive manual operations teams to determine if patients are eligible for care, in-network, based on their payer contracts, and determine the patient’s responsibility towards their healthcare reimbursement. Enter Sohar Health. Our API-based platform streamlines insurance eligibility verification and offers AI-powered Verification of Benefits (VoB) and insurance discovery, automating manual workflows, increasing patient intake, and generating more revenue. Experience the power of seamless integration and unleash the full potential of your behavioral health company with Sohar Health.
🤯 The problem
Improving front end RCM (revenue cycle management) accuracy is crucial as 85% of related-denied claims (worth $40 billion) are preventable. However, determining the eligibility, network status, and pricing transparency for patients is a challenge due to complex relationships between payers and the limited data exchange standards in healthcare IT ecosystem. These exchanges are costly, time-consuming, and divert engineering resources, hindering product development. Delaying or skipping integrations leads to revenue loss and increased manual efforts for RCM operations teams, creating a significant barrier for behavioral health companies in a rapidly growing industry, valued at $280 billion in 2020.
🧠 The Solution
Similar to Stripe (YC09) and Plaid, Sohar Health empowers developers by providing direct integrations to payers. Our API-based platform offers three key features: targeted insurance eligibility determination, accurate network status, and AI-powered Verification of Benefits (VoB). By leveraging our services, behavioral health providers can:
- Unlock up to 25% additional revenue through improved front end RCM accuracy
- Find more eligible patient and minimize churn or attrition
- Halve the time spent on manual operations by intake or RCM teams
👋 Our Backstory
At Pelago (formerly, Quit Genius W18), the leading digital clinic for substance addictions, Ash and Lucas joined forces. Ash is an MD, with a background in digital health, hospital administration, and Health IT strategy consulting. As CTO and employee one at Pelago, Lucas possesses unparalleled expertise in resolving behavioral health integration challenges. With a track record of successfully integrating with 100+ employers, including major players like Evernorth and a Fortune 10 customer, Lucas's firsthand experience and Y Combinator background have been instrumental in securing over $80M in investment funding from seed to Series-B.
Our ask
Introduce us to behavioral health providers (digital or hybrid) in your network. Click here
Connect us to your health plan or payers (e.g. Humana, Cigna, Aetna) that you’re working with. Click here
Interested in hearing more? Feel free to book a meeting here